

About Me
My introduction
A leading Uro-oncologist and Robotic Surgeon at Max Healthcare’s renowned Max Smart Super Speciality Hospital in Saket, New Delhi, Dr. Tushar Aditya Narain represents the pinnacle of advanced urological cancer care. Uniquely trained at University College London Hospital, he brings international expertise in robotic surgical interventions for complex urological cancers. With a distinguished academic background from AIIMS, Delhi and PGI Chandigarh, and an impressive research portfolio of over fifty peer-reviewed publications, Dr. Narain seamlessly bridges innovative surgical techniques with deep academic insights delivering comprehensive, compassionate patient-centered care, setting new standards in urological oncology.

My Degrees
Educational Degrees
- MBBS – Seth GS Medical College and KEM Hospital, Mumbai
- MS General Surgery – All India Institute of Medical Sciences, New Delhi
- MCh Urology – Post Graduate Institute of Medical Education and Research, Chandigarh
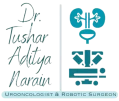
- Clinical Observership Robotic Uro-oncology – Ichan School of Medicine and Mt Sinai Hospital, New York, United States of America
- Fellowship in Robotic Pelvic Uro-oncology – University College London Hospital and NHS Foundation Trust, London, United Kingdom
- AUA Chakrobortty Fellow, Single Port Robotic Surgery, Cleveland Clinic, Ohio, USA
Experience
12 years
Patients Everyday
50+ patients
Diagnosis Daily
50+ patients
Conditions Treated
Providing comprehensive care in
PROSTATE CANCER

PROSTATE CANCER
Prostate cancer is one of the most common malignancies affecting the elderly male. Almost 1 in 10 males would be affected by it in their lifetime. It generally affects males after the age of 50 years but men with a family history of prostate cancer can be affected even at a much younger age. Diagnosing this cancer at its initial stages is of extreme importance, like in any other cancer, but more so in prostate cancer as it provides a window for complete cure from this cancer and normal life expectancy following radical therapy for early stages.
Most of these cancers are asymptomatic to begin with in their earlier stages. However, the common presenting symptoms with which patients come to us are new onset difficulty in passing urine, poor urinary stream, frequent urination, blood in urine, urinary retention and back aches or bony pains, the latter seen in advanced and metastatic stages of the disease. A simple blood test called the Prostate Specific Antigen test can indicate whether the patient has prostate cancer or not and this can be confirmed with a histopathological examination, also known as the biopsy of the prostate. The biopsy is usually done through the rectal passage under ultrasound guidance and is a day care procedure. A MRI and a PSMA PET scan also helps in picking up this cancer and in staging the disease.
Treatment depends on the stage of the disease. Localized prostate cancer can be totally cured with surgery which is now performed using a robot. Robotic radical prostatectomy provides a minimally invasive approach for treating prostate cancer in which the whole prostate along with seminal vesicles are taken out and the patient is usually discharged the next day of the surgery. The blood loss during a robotic surgery is minimal as compared to an open procedure. The recovery is hastened by the avoidance of large incisions, as just five small keyholes are made for the whole surgery. The functional outcomes for the patient, which are the return of urinary continence and preservation of erections are excellent as the robot allows a very meticulous surgery to be performed owing to its magnified 3-D vision during the surgery. Robotic surgery has become the gold standard approach for surgically treating localized prostate cancer as it allows our patients to return to their day to day activities within a couple of days. Most of the patients would be completely treated with surgery alone and would not require any additional therapy apart from a regular follow up with Serum PSA levels. Patients with locally advanced disease may require adjuvant hormone and radiation therapy after the surgical removal of the prostate depending upon the final histopathology report.
Patients with metastatic and advanced disease require hormone therapy in the form of three monthly injections or removal of their testes along with other anti-androgen therapies and chemotherapy. Newer drugs such as abiraterone and enzalutamide have brought about a paradigm shift in the landscape of management of advanced disease and promise hope to these patients.
BLADDER CANCER
BLADDER CANCER
Bladder cancer generally presents in the ageing male, but in the last two decades, the incidence in young adults including ladies has risen alarmingly. Bladder cancer is one of the most lethal of all urological malignancies, second only to kidney cancer in terms of mortality. Smoking constitutes one of the most important risk factors for developing this cancer. Other risk factors include exposure to industrial chemicals, specially those involved in the petrochemical and plastics industry. The most common symptom is blood in urine, scientifically known as hematuria. Other symptoms can be of increased frequency of urination, pain while passing urine, and loss of appetite and weight. Advanced metastatic disease may present with bony pains, cough, breathlessness and blood in sputum.
Initial diagnosis is made with the help of a Ultrasound scan which can be easily done nowadays. Confirmation of the size and location of the tumor is done with the help of a dedicated CT scan. What follows next is an endoscopic surgery called Trans Urethral Resection of Bladder Tumor (TURBT) which removes all of the tumor from the bladder and provides tissue for histopathological examination and biopsy, which establishes the type, grade and stage of tumor. This surgery is done under anaesthesia and is done through the natural orifice of urine, and does not require any cuts or incisions. Patients are generally sent home one to two days after the surgery.
Further treatment depends on the stage of the disease as determined by the biopsy report. A PET scan is done (for muscle invasive disease) to assess if there are any distant metastases or if the tumor is just localized to the bladder. Initial stages, which is the non muscle invasive stage, require instillation of BCG or a chemotherapeutic agent in the bladder along with cystoscopic surveillance. This intravesical therapy prevents the tumor from recurring and progressing. The drug is initially instilled weekly for 6 weeks, which is the induction course, followed by monthly instillations, which is the maintenance regimen. The maintenance regimen goes on The more advanced stage, which is the muscle invasive, stage requires a radical surgery which involves removal of the whole bladder, besides the prostate in the males and uterus, cervix and fallopian tubes in females. The bladder is replaced by an orthotopic neo bladder or an ileal conduit which is made from the small intestine. Robotic surgery allows a minimally invasive approach for this major surgery wherein the patient does not have any big incisions on his abdomen and gets up and walks about the next day of the surgery as opposed to a traditional open approach which involves a large incision prolonging patient recovery. Patients not fit for anaesthesia and surgery are offered radiotherapy and chemotherapy with a curative intent. Follow up after surgery involves regular visits to your doctor for physical examination, routine blood tests and a cross sectional imaging such as a CT scan. Patients with metastatic disease are treated with systemic chemotherapy and immunotherapy.
KIDNEY CANCER
KIDNEY CANCER
Renal cancers arise in patients generally aged beyond 60, both in males and females and commonly present with blood in urine, pain in abdomen, or a lump in abdomen which is seen in more advanced stages. However about 60 % of the patients diagnosed with renal cancer are asymptomatic, and detected to have the lesion on an abdominal ultrasound done for an unrelated reason. The major risk factor for development of renal cancer is tobacco exposure, mainly in the form of smoking. The risk almost doubles with every 10 years of smoking. Other risk factors include obesity, hypertension, chronic NSAID painkiller use and some industrial chemical exposure. Renal tumours are diagnosed and characterised by abdominal CT scans. The mainstay of treatment of these tumours are surgical removal, either removal of the whole kidney, known as radical nephrectomy, or just removal of the tumour while preserving the rest of the kidney in the case of small masses, known as partial nephrectomy. Minimally invasive approach in the form of robotic surgery or laparoscopic surgery is the preferred form of surgery and avoids the morbidity of a large incision of an open surgery. The robotic approach also makes possible removal of large complex tumors while preserving the rest of the kidney, which was not possible earlier with the conventional laparoscopic approach. Patients with metastatic and advanced disease are treated with targeted therapy with Tyrosine Kinase inhibitors or with the newer immunotherapeutic agents.
TESTICULAR CANCER
TESTICULAR CANCER
Testicular cancer usually presents with painless enlargement of the testis. Attention is drawn towards an enlarging testes usually after a trivial trauma. There is associated decrease in sensation of the afflicted testes. Testicular tumors are broadly divided into two categories, the semonomatous and the non-seminomatous types. The age of presentation, prognosis and treatment modalities differ for these two types of tumor. Distinction amongst these two types of tumor is made initially by the blood levels of Alpha feto protein (AFP), Beta Human Chorionic Gonadotropin (B-HCG) levels and Lactate dehydrogenase (LDH) levels. Final diagnosis is made by histopathological examination following a high inguinal orchidectomy. Transcrotal biopsy or a scrotal orchidectomy is not recommended owing to oncological reasons. Staging is done using CT scans of the chest and the abdomen to detect metastases to the retroperitoneum nodes. Treatment depends on the stage of the disease and the type of tumor (Seminoma vs Non Seminoma) and levels of blood markers. Initial stages are managed with high inguinal orchidectomy followed by surveillance while the more advanced stages need chemotherapy and surgery (Retroperitoneal Lymph Node Dissection (RPLND)) or radiotherapy depending upon the tumor subtype. RPLND can be done using robotic approach providing the benefits of a minimally invasive approach as against an open approach for this major surgery.
PENILE CANCER
PENILE CANCER
Penile cancer presents with a growth, usually involving the glans or the prepuce of the penis. Uncircumcised males with poor hygiene are at high risk of developing a lesion, and circumcision is protective against penile cancers. The Human Papilloma Virus, responsible for cervical cancers in females, are also a causative factor for development of penile cancer. A warty growth on the glans is the most common presentation, while earlier stages might present with discolouration or a patch on the glans and the more advanced stages present with a cauliflower like growth replacing a part or the whole of the penis. Some patients also have swelling and ulcers in the inguinal region on one or both sides at presentation, representing more advanced stages of the disease. Diagnosis is based on clinical examination and a CT scan of the chest, abdomen and pelvis to detect metastases. A wedge biopsy of the lesion confirms the diagnosis and the final treatment depends on the stage of the disease. Smaller lesions can be treated with partial excision of the glans or partial amputation of the penis. Larger growths require a radical penectomy or removal of the whole penis and creation of perineal urethrostomy. Most of the patients also require a bilateral inguinal and pelvic lymph node dissection which is done by robotic approach. Larger inoperable tumors can be treated with radiotherapy and metastatic disease is treated with systemic cytotoxic chemotherapy.
ADRENAL CANCER
ADRENAL CANCER
Adrenal tumours can either be benign tumors, adrenal cortical cancers or paraganglioma arising from the adrenal medulla known as pheochromocytomas. Tumors arising from the cortex of the adrenal, whether benign or adrenal cortical carcinoma, are usually asymptomatic, but may present with abdominal pain or a lump in cases of large masses. Some of these tumors also produce excess steroids and sex hormones and patients may present with symptoms arising from these excess production of the hormones. Patients with pheochromocytomas present with symptoms of catecholamine excess, the classical triad being headache, palpitation and excessive sweating. Hypertension and deranged glucose metabolism also results for excess production of catecholamine. Diagnosis is made based on CT scan of the abdomen and measurement of plasma metanephrine and nor metanephrine levels. Surgery is the mainstay of treatment for adrenal masses, for both cortical tumors and of pheochromocytomas, albeit pheochromocytomas require medical counteraction of the effects of excessive catecholamine before surgery. Robotic and laparoscopic approach provide a minimally invasive means of removal of the tumor with minimal morbidity as against an open approach.
Surgeries Performed
Surgical operation in

Robot Assisted Radical Prostatectomy (RALP)

Robot Assisted Radical Cystectomy with Intracorporeal Neo-Bladder (RARC + ONB)

Robot Assisted Radical Cystectomy with Intracorporeal Ileal Conduit (RARC + IC)

Robot Assisted Radical Nephrectomy

Robot Assisted Partial Nephrectomy/ Robot Assisted Nephron Sparing Surgery (RA-NSS)

Robot Assisted Retroperitoneal Lymph Node Dissection (RPLND)

Robot Assisted Video Endoscopic Inguinal Lymph Node Dissection (VEIL)

Robotic Adrenalectomy

Open/Laparoscopic Radical Nephrectomy

Endourological Procedure
My Team

Mr. Praveen Rathi
Robotic Physician Assistant
Urooncology and Robotic Surgery
Max Institute of Cancer Care

Mr. Manish Sharma
Urooncology and Prostate Cancer CNS
Urooncology and Robotic Surgery
Max Institute of Cancer Care

Mr. Manpreet Singh
Program Coordinator
Urooncology and Robotic Surgery
Max Institute of Cancer Care

Dr. Naresh Kaul
MBBS MS MCh
Fellowship in Urooncology and Robotic Surgery
Consultant, Urooncology and Robotic Surgery
Max Smart Super Speciality Hospital Saket
Research Papers
My academic work

Pelvic Lymph Node Dissection at the Time of Radical Prostatectomy: Extended? Of Course Not!

Neoadjuvant Therapy for Cisplatin Ineligible Muscle Invasive Bladder Cancer Patients: A Review of Available Evidence
Expert Recommendations
What my mentors say

Mr. Greg Shaw
Consultant Urological Surgeon, Clinical Lead for Robotic Surgery and Pelvic Uro-oncology, University College London Hospital, London
"Tushar has been an excellent robotic fellow for two years at UCLH, London and has worked hard and learnt a great deal. He has been a key part of the largest robotic pelvic surgery team in the UK. He has excellent operative skills and I am very confident that he will provide a very high level of care for his patients as a consultant in India."

Prof. Arup Kumar Mandal
Professor, Department of Urology
All India Institute of Medical Sciences (AlIMS), Rishikesh
Former Professor & Chairman
Department of Urology. PGIMER, Chandigarh
"I have known Tushar for several years now and having worked with him both at PGI, Chandigarh and at AlIMS, Rishikesh, I can vouch for the fact that he is not only a very competent surgeon, but he also deals with his patients with utmost compassion and care."

Mr. Senthil Nathan
MBBS, MS, FRCS, DUrol
Director of Robotic Surgery & Surgical Innovations, Chair of MDT, Consultant Urologist Cleveland Clinic
London
"It was an immeasurable joy to mentor Tushar for two years at UCLH, London to become an accomplished robotic surgeon. He was keen, eager, adaptive and always available to strive for the team. From a novice he became an expert in Robotic Uro-oncology with platitude and stability. He will always be a great asset to any institution he joins and a dear colleague to have. I opened the door but Tushar entered by himself; "there was no need to teach an eagle to fly."

Professor Prasanna Sooriakumaran
MD PhD FRCSUrol FEBU
Professor and Chair of Urology
Cleveland Clinic London
"Tushar is an exceptional doctor, a well rounded surgeon with strong robotic skills and great at managing patients. I am proud to have trained him in my techniques of robotic prostatectomy including nerve sparing, Retzius sparing, and other advanced methods to help patients recover their urinary continence and erections after curative prostate cancer surgery. I would thoroughly recommend Tushar to any patient who has any urology problems, especially if it is cancer. You will be in great hands!"